Perspective
Foodborne Disease in 2011 — The Rest of the Story
NEJM February 23, 2011 Topics: Drugs, Devices, and the FDA, Public Health
Michael T. Osterholm, Ph.D., M.P.H.
Recent media headlines might have you believe that our food supply is substantially more safe than it was a decade ago and about to get even safer. First, on December 15, 2010, the Centers for Disease Control and Prevention (CDC) announced a long-awaited reanalysis of the burden of foodborne illness in the United States and reported a substantial decrease in the estimated incidence of foodborne disease between 1999 and 2011. Then, on January 4, 2011, President Barack Obama signed into law the Food Safety Modernization Act, the first major legislation related to the food-safety authority of the Food and Drug Administration (FDA) since 1938. But as the late radio commentator Paul Harvey would say, “You know what the news is; in a minute, you’re going to hear . . . the rest of the story.”
As the first set of headlines indicated, the CDC reported a substantial decrease in the estimated incidence of foodborne disease between 1999 and 2011. In 1999, Mead and colleagues published the first comprehensive estimates of foodborne disease in the United States.1 Scallan and colleagues, in two recent articles, detail new estimates of the burden of foodborne disease for 31 known2 and unspecified3 infectious agents. In 1999, it was estimated that annually, foodborne pathogens caused 76 million episodes of illness, 325,000 hospitalizations, and 5000 deaths. On the basis of these estimates, 27% of Americans could expect to have a foodborne illness each year, 115 per 100,000 population would be hospitalized, and almost 2 per 100,000 would die.
The CDC now estimates that there are approximately 48 million foodborne illnesses, 128,000 hospitalizations, and 3000 deaths per year.
That means that 15% of Americans can expect to have a foodborne illness annually and that 41 in 100,000 will be hospitalized and 1 in 100,000 will die. However, the authors have strongly cautioned that the 1999 estimates cannot be compared with the current ones for purposes of trend analysis, because different methods and underlying assumptions were used.
Therefore, we cannot draw inferences from these CDC data about the relative safety of our food supply today, as compared with 12 years ago.
More reliable trend data for disease incidence are available from the Foodborne Disease Active Surveillance Network (FoodNet) of the CDC’s Emerging Infections Program. FoodNet supports active, population-based surveillance in 10 states for all laboratory-confirmed infections with selected pathogens that are commonly transmitted through food.4 The system has been in place since 1996. It provides a relatively constant measuring stick of the incidence of foodborne disease across geographic areas and over time. Additional data that are collected by local and state health departments participating in FoodNet also help to define routes of exposure to various foodborne pathogens, in part by identifying the roles played by food not typically associated with outbreaks of foodborne disease and food preparation in the risk of disease. These data show that even with improvements made during the past decade, the burden of foodborne disease persists.
According to a 2010 FoodNet report, which included preliminary data from 2009, rates of infection with shigella, yersinia, Shiga-toxin–producing Escherichia coli (STEC) O157, campylobacter, and listeria were at least 25% lower than they were a decade ago; the rate of infection with salmonella, a bellwether pathogen for foodborne-disease surveillance, was only 10% lower.
Rates of vibrio infection were substantially higher in 2009 than in the period from 1996 through 1998.4 All these findings, however, must be interpreted with caution, since most of the decreases occurred between 1996 and 2000, and there has been little additional change since then. When the 2009 incidence of infections with the eight primary bacterial and parasitic pathogens is compared with their incidence in the period from 2006 through 2008, no significant change can be seen for six pathogens; only the infection rates with shigella and STEC O157 show significant decreases (see graph).
In addition, recent studies have demonstrated a significant increase in the incidence of foodborne disease caused by emerging non-O157 STEC, suggesting that surveillance for O157 is no longer sufficient to determine the effect of foodborne STEC infections.
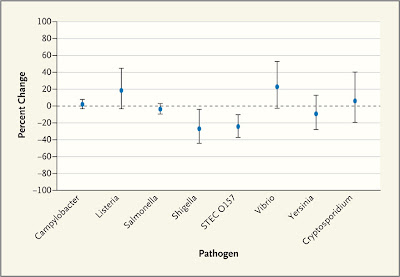
Percent Change in the Incidence of Laboratory-Confirmed Bacterial and Parasitic Infections from 2006–2007 to 2009, According to Pathogen.
On the basis of FoodNet data for the past 14 years, we must conclude that the improvements made in the late 1990s in the safety of our food supply are still having a positive effect. But we’ve made little additional progress in the past decade. Although the media and some food producers, processors, wholesalers, and retailers may conclude that the recent CDC estimates offer evidence of major improvements in food safety since 1999, data from active population-based surveillance offer a more nuanced and neutral picture. Moreover, in this issue of the Journal, Barton Behravesh et al. remind us that previously unrecognized vehicles for foodborne disease, such as jalapeño peppers, can cause large nationwide outbreaks. And outbreaks associated with raw produce are among the most difficult ones for public health officials to identify and control, since produce from a single farm may be distributed widely and consumed rapidly because it is perishable.
So will the Food Safety Modernization Act result in immediate improvements in food safety? The legislation brings long overdue modernization to the FDA’s food-safety activities. It gives the FDA broader authority to regulate food facilities, including authorization to inspect records related to food. It “requires each owner, operator, or agent in charge of a [nonexempt] food facility to identify and implement preventive controls to significantly minimize or prevent hazards that could affect food manufactured, processed, packed, or held by [that] facility.” It also requires the FDA “to issue guidance documents to reduce the risk from the most significant foodborne contaminants” and to “establish minimum standards for the safe production and harvesting of fruits and vegetables based on known safety risks.” It further requires the FDA “to allocate resources to inspect facilities and imported food according to the known safety risks of the facilities or food; and [to] establish a product tracing system to track and trace food that is in the United States or offered for import into the United States.” It gives the FDA authority to order a recall of a food when it is contaminated or implicated in an outbreak.
.
Finally, it “requires U.S. importers to perform risk-based foreign supplier verification activities to verify that imported food is produced in compliance with applicable requirements related to hazard analysis and standards for produce safety and is not adulterated or misbranded.”
Although all these new forms of authority will substantially enhance the FDA’s ability to prevent foodborne disease and respond more effectively when an outbreak occurs, the new law has a major shortcoming: dollars. There was no appropriation approved by the Congress for the act or authorization in the bill for the FDA to assess fees on the companies that it inspects. The Congressional Budget Office estimated that implementing this legislation would require $1.4 billion between 2011 and 2015.5 Though the bill authorizes the FDA to collect fees when a facility requires reinspection and a recall fee for mandatory recalls, these fees are expected to provide minimal resources.
Although all these new forms of authority will substantially enhance the FDA’s ability to prevent foodborne disease and respond more effectively when an outbreak occurs, the new law has a major shortcoming: dollars. There was no appropriation approved by the Congress for the act or authorization in the bill for the FDA to assess fees on the companies that it inspects. The Congressional Budget Office estimated that implementing this legislation would require $1.4 billion between 2011 and 2015.5 Though the bill authorizes the FDA to collect fees when a facility requires reinspection and a recall fee for mandatory recalls, these fees are expected to provide minimal resources.
.
In short, the actual effect of this important law will at best be extremely limited if Congress and the administration don’t appropriate and sign additional legislation providing the necessary funds to carry out its mandates. Recent reports in the media calling this act “historic legislation” must be tempered by the reality that without the necessary resources, requiring the FDA to carry out the law’s required activities will be like trying to get blood out of a rock. And in the end, food safety in the United States cannot be expected to improve in more than an incremental manner.
As Paul Harvey would have said, “That’s the rest of the story.”
This article (10.1056/NEJMp1010907) was published on February 23, 2011, at NEJM.org.
Disclosure forms provided by the author are available with the full text of this article at NEJM.org .
Source Information
From the Center for Infectious Disease Research and Policy, University of Minnesota, Minneapolis.
References
Mead PS, Slutsker L, Dietz V, et al. Food-related illness and death in the United States. Emerg Infect Dis 1999;5:607-625CrossRef Web of Science Medline
Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States — major pathogens. Emerg Infect Dis 2011;17:7-15Medline
Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States — unspecified agents. Emerg Infect Dis 2011;17:16-22Medline
Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food — 10 states, 2009. MMWR Morb Mortal Wkly Rep 2010;59:418-422Medline
Congressional Budget Office. Senate File 510: Food Safety Modernization Act — as reported by the Senate Committee on Health, Education, Labor, and Pensions. August 12, 2010.
Mead PS, Slutsker L, Dietz V, et al. Food-related illness and death in the United States. Emerg Infect Dis 1999;5:607-625CrossRef Web of Science Medline
Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States — major pathogens. Emerg Infect Dis 2011;17:7-15Medline
Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States — unspecified agents. Emerg Infect Dis 2011;17:16-22Medline
Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food — 10 states, 2009. MMWR Morb Mortal Wkly Rep 2010;59:418-422Medline
Congressional Budget Office. Senate File 510: Food Safety Modernization Act — as reported by the Senate Committee on Health, Education, Labor, and Pensions. August 12, 2010.
No comments:
Post a Comment